1. Male Reproductive System: Overview
The male reproductive system consists of primary and accessory organs responsible for producing, storing, and transporting sperm. It also plays a role in hormone secretion, particularly testosterone, which regulates secondary sexual characteristics. The primary sex organs are the testes, which produce sperm and hormones. The accessory organs include the duct system, glands, and external genitalia, which assist in the transportation, nourishment, and delivery of sperm.
2. Components of the Male Reproductive System
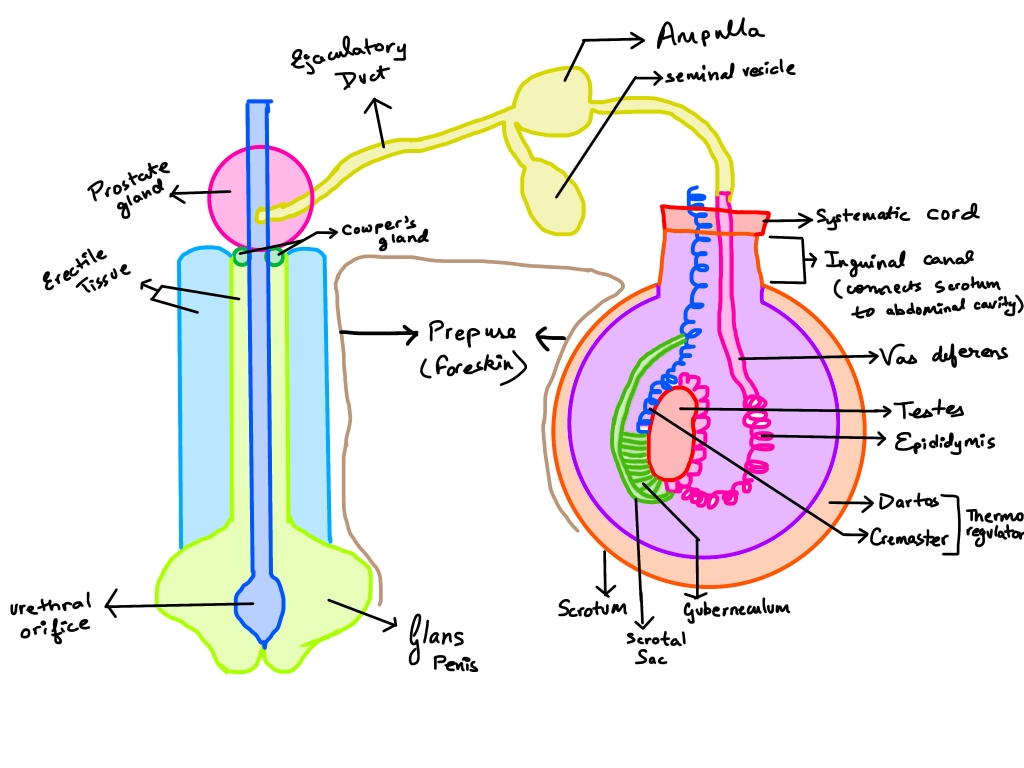
✅ A. Testes (Primary Organ)
The testes are a pair of oval-shaped organs located in the scrotum, outside the abdominal cavity.
- Structure: Each testis is covered by a tough connective tissue capsule called the tunica albuginea. Internally, the testis contains seminiferous tubules, which are the site of sperm production.
- Function:
- Spermatogenesis: The seminiferous tubules contain germ cells that differentiate into sperm.
- Hormone Secretion: The Leydig cells (interstitial cells) between the tubules produce testosterone, which regulates sperm production and secondary sexual characteristics.
- Temperature Regulation: The scrotum maintains the testes at a temperature 2–3°C lower than the body temperature, which is essential for proper sperm production.
✅ B. Scrotum
The scrotum is a pouch of skin and muscle located outside the body that contains and protects the testes.
- Structure: It is divided into two compartments by a septum. Each compartment holds one testis. The dartos muscle (smooth muscle) and cremaster muscle (skeletal muscle) help regulate the position of the testes.
- Function:
- Temperature Regulation: The scrotum maintains an optimal temperature for spermatogenesis by contracting and relaxing the cremaster muscle to move the testes closer to or away from the body.
- Protection: It provides a protective covering for the testes, shielding them from external injury.
✅ C. Epididymis
The epididymis is a coiled tube situated at the back of each testis. It is divided into three parts: head, body, and tail.
- Structure: The head receives immature sperm from the seminiferous tubules. The body and tail store and transport sperm.
- Function:
- Sperm Maturation: Sperm gain motility and fertilizing ability as they pass through the epididymis.
- Sperm Storage: The tail serves as a reservoir where mature sperm are stored until ejaculation.
- Conduction: During ejaculation, the epididymis contracts to propel sperm into the vas deferens.
✅ D. Vas Deferens (Ductus Deferens)
The vas deferens is a muscular tube that connects the epididymis to the ejaculatory duct.
- Structure: It is a thick-walled, muscular duct approximately 30–45 cm long. It runs from the scrotum, through the inguinal canal, and into the pelvic cavity.
- Function:
- Sperm Transport: During ejaculation, rhythmic contractions of the muscular wall of the vas deferens propel sperm toward the urethra.
- Temporary Storage: It can store sperm for a short duration.
- Contribution to Seminal Fluid: It mixes sperm with secretions from the seminal vesicles and prostate gland to form semen.
✅ E. Seminal Vesicles
The seminal vesicles are a pair of elongated glands located behind the bladder.
- Structure: Each gland is about 5 cm long and has a honeycomb-like interior lined with columnar epithelium.
- Function:
- Secretion of Seminal Fluid: They produce a fructose-rich fluid that nourishes sperm and enhances their motility.
- Volume of Semen: Their secretion makes up about 60-70% of the semen volume.
- Alkalinity: The fluid is alkaline, which helps neutralize the acidic environment of the female reproductive tract, aiding sperm survival.
✅ F. Prostate Gland
The prostate gland is a walnut-sized gland located below the bladder, surrounding the upper part of the urethra.
- Structure: It consists of tubuloalveolar glands embedded in a fibromuscular stroma.
- Function:
- Secretion of Prostatic Fluid: It produces a milky, slightly acidic fluid that forms about 20-30% of the semen volume. This fluid contains citrate, zinc, and enzymes, which enhance sperm motility.
- PSA Enzyme: The gland secretes prostate-specific antigen (PSA), which liquefies semen, making it easier for sperm to swim.
- Neutralizing Acidic Urine: It prevents the acidic remnants of urine from damaging sperm during ejaculation.
✅ G. Bulbourethral Glands (Cowper’s Glands)
The bulbourethral glands are two pea-sized glands located below the prostate gland, near the base of the penis.
- Structure: These glands are made of tubuloalveolar tissue and have ducts that open into the urethra.
- Function:
- Pre-ejaculatory Fluid: They secrete a clear, slippery fluid that lubricates the urethra and neutralizes traces of acidic urine.
- Sperm Protection: This fluid forms part of the pre-ejaculate and provides a suitable environment for sperm.
✅ H. Urethra
The urethra is a tube that carries both urine and semen out of the body through the penis.
- Structure: It is divided into three regions:
- Prostatic urethra: Passes through the prostate gland.
- Membranous urethra: Narrowest part, surrounded by the external urethral sphincter.
- Spongy urethra: Runs along the length of the penis and opens at the external urethral orifice.
- Function:
- Urine and Semen Passage: It serves as a common conduit for the expulsion of urine and semen.
- Protection: During ejaculation, the internal urethral sphincter closes to prevent the backflow of semen into the bladder.
✅ I. Penis
The penis is the external genital organ involved in copulation and the passage of urine.
- Structure: It consists of three erectile tissues:
- Two corpora cavernosa (dorsal) and one corpus spongiosum (ventral), which surrounds the urethra.
- The glans penis is the sensitive tip, covered by a fold of skin called the prepuce.
- Function:
- Erection: During sexual arousal, blood fills the erectile tissues, causing an erection, which facilitates penetration.
- Semen Ejaculation: The penis serves as the delivery organ for sperm during intercourse.
- Urination: It also functions as a conduit for urine elimination.
✅ J. Semen (Ejaculate)
Semen is a mixture of sperm and secretions from accessory glands.
- Components:
- Sperm (10%)
- Seminal vesicle fluid (60-70%)
- Prostate gland fluid (20-30%)
- Bulbourethral gland secretions (small amount)
- Function:
- Transport Medium: It provides a fluid medium for sperm transportation.
- Nutrition and Protection: It contains fructose, proteins, and enzymes that nourish and protect sperm.
- pH Balance: Its alkaline nature neutralizes vaginal acidity, increasing sperm survival.
3. Female Reproductive System: Overview
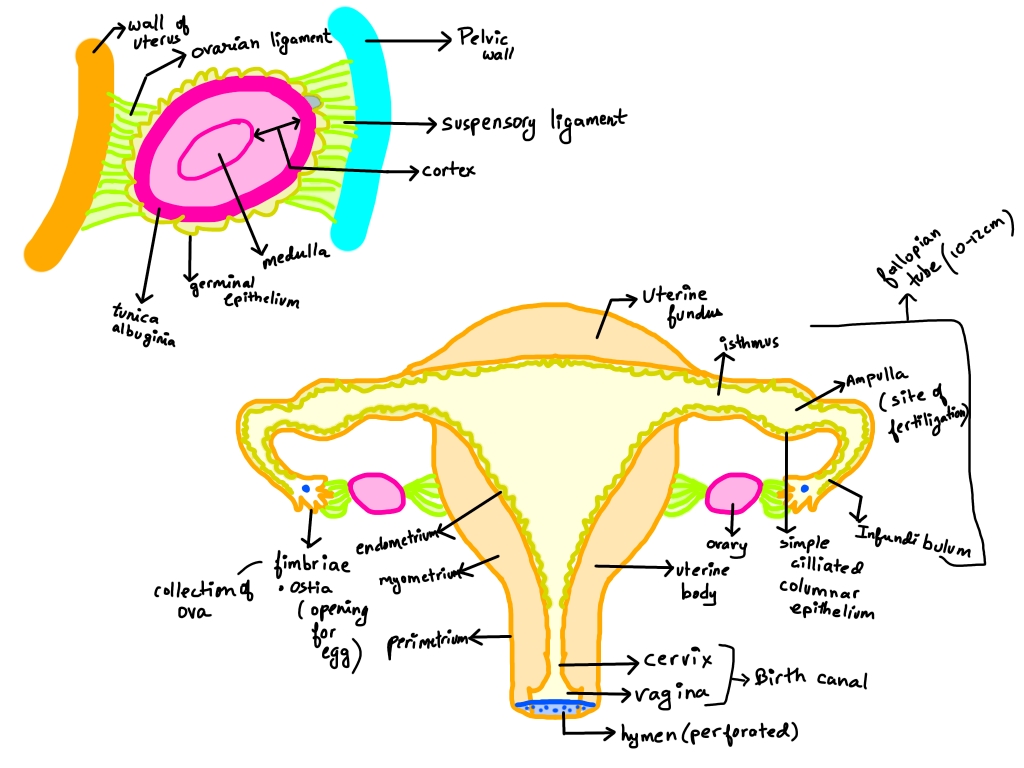
The female reproductive system is responsible for the production of ova (eggs), fertilization, and providing an environment for the development of the embryo and fetus. It consists of primary reproductive organs (ovaries) and accessory organs, which include the fallopian tubes, uterus, cervix, vagina, and external genitalia. The system also contains glands that contribute to lubrication and support reproductive processes.
4. Components of the Female Reproductive System
✅ A. Ovaries (Primary Organ)
The ovaries are a pair of small, oval-shaped glands located in the lower abdominal cavity, on either side of the uterus.
- Structure:
- Each ovary is about 2-4 cm in length and consists of two regions:
- Cortex: Contains ovarian follicles at different stages of development.
- Medulla: Contains blood vessels, lymph vessels, and nerves.
- Function:
- Oogenesis: Ovaries produce and release mature ova (eggs) during the menstrual cycle.
- Hormone Secretion: They secrete estrogen and progesterone, which regulate menstrual cycles, secondary sexual characteristics, and pregnancy.
- Ovulation: The Graafian follicle ruptures during ovulation, releasing the egg into the fallopian tube.
✅ B. Fallopian Tubes (Oviducts)
The fallopian tubes are a pair of muscular tubes extending from the ovaries to the uterus. They serve as the site of fertilization.
- Structure:
- Each tube is about 10-12 cm long and has four regions:
- Infundibulum: Funnel-shaped, located near the ovary with fimbriae that sweep the egg into the tube.
- Ampulla: Widest section where fertilization usually occurs.
- Isthmus: Narrow portion that connects to the uterus.
- Uterine part: Opens into the uterine cavity.
- Function:
- Egg Transport: The ciliated epithelium and muscular contractions move the egg toward the uterus.
- Fertilization Site: The ampulla is the most common site of fertilization.
- Early Embryo Transport: The fertilized zygote is transported to the uterus for implantation.
✅ C. Uterus (Womb)
The uterus is a pear-shaped, hollow muscular organ located in the pelvis, between the bladder and rectum. It is the site where the embryo implants and develops during pregnancy.
- Structure:
- The uterus has three layers:
- Perimetrium: Outer serous layer.
- Myometrium: Thick muscular layer responsible for contractions during labor.
- Endometrium: Inner mucosal layer that thickens during the menstrual cycle and is shed during menstruation.
- Function:
- Implantation: The fertilized egg attaches to the endometrial lining.
- Nourishment of the Fetus: The uterus provides vascular and nutrient support to the developing fetus through the placenta.
- Menstruation: In the absence of fertilization, the endometrium is shed during menstruation.
- Contraction During Labor: The myometrium contracts during childbirth to expel the baby.
✅ D. Cervix
The cervix is the narrow, lower portion of the uterus that connects to the vagina. It acts as a gateway between the uterus and the vagina.
- Structure:
- It contains cervical glands that secrete mucus.
- The external os opens into the vagina, and the internal os opens into the uterus.
- Function:
- Secretion of Mucus: Cervical glands produce mucus that changes in consistency during the menstrual cycle to either block or facilitate sperm entry.
- Protection Against Infections: The mucus acts as a barrier against pathogens.
- Dilates During Labor: During childbirth, the cervix dilates up to 10 cm to allow the baby to pass through.
✅ E. Vagina
The vagina is a fibromuscular canal that connects the cervix to the external genitalia. It serves as the copulatory organ and the birth canal.
- Structure:
- It is about 7-10 cm long and has elastic walls capable of expanding during intercourse and childbirth.
- The vaginal wall consists of three layers:
- Mucosa: Inner layer with folds called rugae, which expand during childbirth.
- Muscularis: Middle layer with smooth muscle fibers.
- Adventitia: Outer connective tissue layer.
- Function:
- Receives Semen: Acts as the receptacle for sperm during intercourse.
- Birth Canal: During delivery, the baby passes through the vagina.
- Menstrual Flow Exit: It allows the exit of menstrual blood during menstruation.
✅ F. External Genitalia (Vulva)
The external genitalia include the mons pubis, labia majora, labia minora, clitoris, and vestibular glands.
- Structure:
- Mons pubis: Fatty tissue over the pubic bone, covered with hair after puberty.
- Labia majora: Larger outer folds of skin.
- Labia minora: Smaller inner folds, enclosing the vaginal and urethral openings.
- Clitoris: A small erectile organ with numerous nerve endings.
- Vestibular glands (Bartholin’s glands): Secrete lubricating fluid.
- Function:
- Protection: The labia protect the vaginal and urethral openings from infections.
- Lubrication: The Bartholin’s glands secrete mucus to lubricate the vaginal opening during intercourse.
- Sexual Arousal: The clitoris becomes engorged during arousal, contributing to sexual pleasure.
✅ G. Bartholin’s Glands (Vestibular Glands)
The Bartholin’s glands are two small, pea-sized glands located on either side of the vaginal opening.
- Structure:
- They have small ducts that open near the vaginal orifice.
- Function:
- Lubrication: They secrete a mucous-like fluid during sexual arousal to reduce friction during intercourse.
- Moisture Maintenance: They help keep the vaginal opening moist.
✅ H. Clitoris
The clitoris is a small, erectile organ located at the junction of the labia minora.
- Structure:
- It consists of erectile tissue and has a high concentration of nerve endings, making it highly sensitive.
- Function:
- Sexual Arousal: During arousal, it becomes engorged with blood, enhancing sexual pleasure.
- Sensitive Organ: It plays a key role in sexual sensation and pleasure.
Mammary Glands (Breasts)
The mammary glands are modified sweat glands responsible for milk production during lactation.
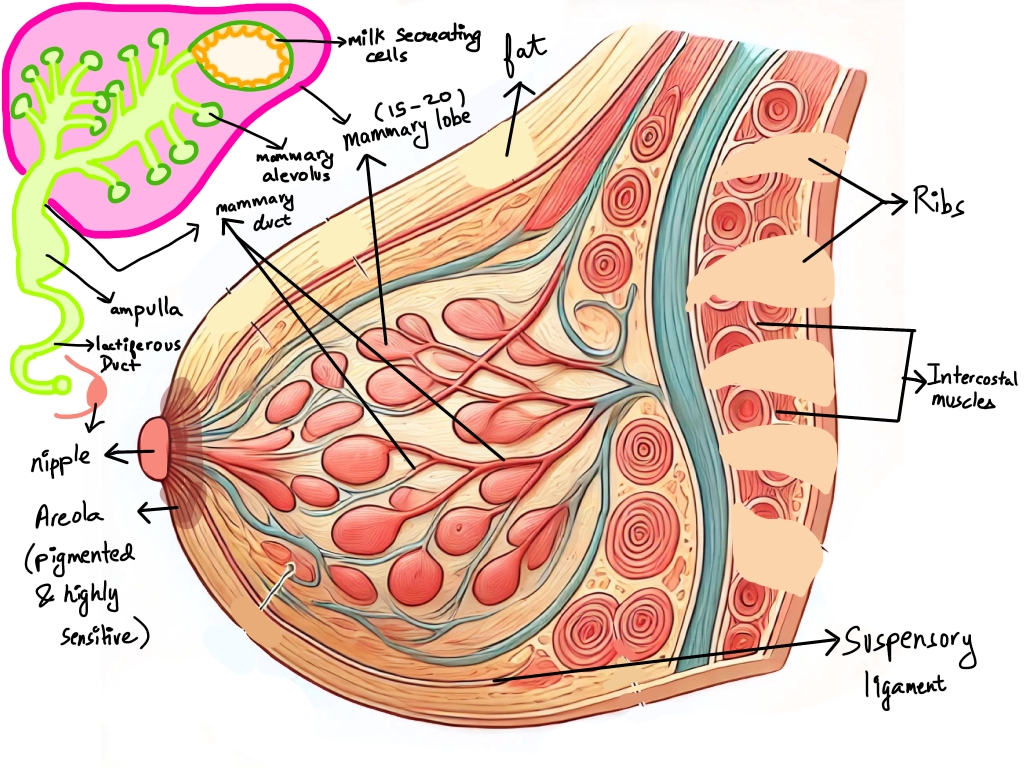
- Structure:
- Each breast contains lobes made of smaller lobules, which contain milk-secreting alveoli.
- The ducts from the lobules open at the nipple, which is surrounded by the areola.
- Function:
- Lactation: After childbirth, the alveoli produce milk under the influence of prolactin, while oxytocinstimulates milk ejection.
- Nutrition: Breast milk provides essential nutrients and antibodies to the newborn.
- Sexual Sensation: The areola and nipple contain nerve endings that contribute to sexual arousal.
✅ 1. Gametogenesis:
Gametogenesis is the biological process by which gametes (sperm and ova) are produced in sexually reproducing organisms through meiotic cell division. It occurs in the gonads (testes in males and ovaries in females) and involves the reduction of chromosome number from diploid (2n) to haploid (n), ensuring that the resulting gametes carry half the genetic material of the parent cells.
- Significance of Gametogenesis:
- Ensures the formation of haploid gametes, which restore the diploid chromosome number during fertilization.
- Introduces genetic variation through crossing over and random assortment of chromosomes during meiosis.
- Produces mature and functional gametes capable of fertilization.
- Main Processes Involved:
- Spermatogenesis: Formation of sperm in males.
- Oogenesis: Formation of ova in females.
✅ 2. Spermatogenesis: Process of Sperm Formation
Spermatogenesis is the process by which spermatogonia (diploid germ cells) in the testes undergo mitotic and meiotic divisions to produce mature spermatozoa (sperm). It occurs in the seminiferous tubules of the testes and is regulated by hormones.
- Phases of Spermatogenesis:
- Multiplication Phase:
- Occurs in the germinal epithelium of the seminiferous tubules.
- Diploid spermatogonia (2n) divide repeatedly by mitosis to form primary spermatocytes (2n).
- This phase increases the pool of precursor cells.
- Growth Phase:
- The primary spermatocytes enlarge and prepare for meiosis.
- No cell division occurs; instead, the cells increase in size and accumulate nutrients.
- Maturation Phase:
- The primary spermatocytes undergo the first meiotic division, producing two haploid secondary spermatocytes.
- The secondary spermatocytes undergo the second meiotic division, forming four spermatids (n).
- Spermiogenesis:
- The spermatids transform into mature spermatozoa (sperm) through morphological changes:
- Formation of acrosome from the Golgi apparatus.
- Development of a flagellum for motility.
- Condensation of nuclear material and shedding of excess cytoplasm.
- Spermiation:
- The release of mature sperm from the Sertoli cells into the lumen of seminiferous tubules.
- The sperm are transported to the epididymis for maturation and storage.
✅ 3. Oogenesis: Process of Ovum Formation
Oogenesis is the process by which ova (egg cells) are produced in the ovaries of females. It begins before birth and continues until menopause. Unlike spermatogenesis, which produces millions of sperm daily, oogenesis produces one ovum per menstrual cycle.
- Phases of Oogenesis:
- Multiplication Phase (Fetal Stage):
- During fetal development, primordial germ cells (2n) undergo repeated mitotic divisions to form oogonia (2n).
- By the fifth month of fetal development, around 6-7 million oogonia are present.
- Most oogonia undergo degeneration (atresia), and only around 1-2 million primary oocytes remain at birth.
- Growth Phase (Before Puberty):
- The surviving oogonia enlarge to form primary oocytes.
- Each primary oocyte is surrounded by a layer of granulosa cells, forming a primary follicle.
- The primary oocytes enter prophase-I of meiosis but remain arrested until puberty.
- Maturation Phase (After Puberty):
- During each menstrual cycle, a primary oocyte completes meiosis-I, producing two unequal cells:
- A secondary oocyte (n) with most of the cytoplasm.
- A first polar body (n), which is non-functional.
- The secondary oocyte begins meiosis-II but is arrested at metaphase-II until fertilization.
- During fertilization, meiosis-II is completed, forming a haploid ovum (n) and a second polar body.
- Differences from Spermatogenesis:
- Oogenesis produces one ovum and three polar bodies, whereas spermatogenesis produces four functional sperm.
- Oogenesis begins before birth, while spermatogenesis starts at puberty.
✅ 4. Hormonal Control of Spermatogenesis
Spermatogenesis is regulated by a complex interaction of hormones produced by the hypothalamus, pituitary gland, and testes.
- Hormones Involved:
- Gonadotropin-Releasing Hormone (GnRH):
- Secreted by the hypothalamus.
- Stimulates the anterior pituitary gland to release FSH and LH.
- Follicle-Stimulating Hormone (FSH):
- Acts on Sertoli cells in the seminiferous tubules.
- Stimulates the production of androgen-binding protein (ABP), which maintains a high testosterone concentration in the testes, essential for spermatogenesis.
- Promotes nourishment and support of developing sperm cells.
- Luteinizing Hormone (LH):
- Stimulates Leydig cells in the testes.
- Induces the production of testosterone, which is necessary for sperm maturation.
- Testosterone:
- Secreted by Leydig cells under the influence of LH.
- Maintains the growth and development of the male reproductive system.
- Stimulates the final stages of spermatogenesis.
- Responsible for the development of secondary sexual characteristics.
- Inhibin:
- Produced by Sertoli cells.
- Acts on the pituitary gland to inhibit FSH secretion when sperm production is sufficient, thus regulating spermatogenesis.
- Feedback Mechanism:
- Negative Feedback Loop:
- High testosterone levels inhibit the secretion of GnRH and LH, regulating sperm production.
- Inhibin reduces FSH secretion, preventing overproduction of sperm.
✅ 5. Structure of Sperm
Sperm is a haploid male gamete produced in the testes. It is a motile cell specialized for fertilizing the ovum.
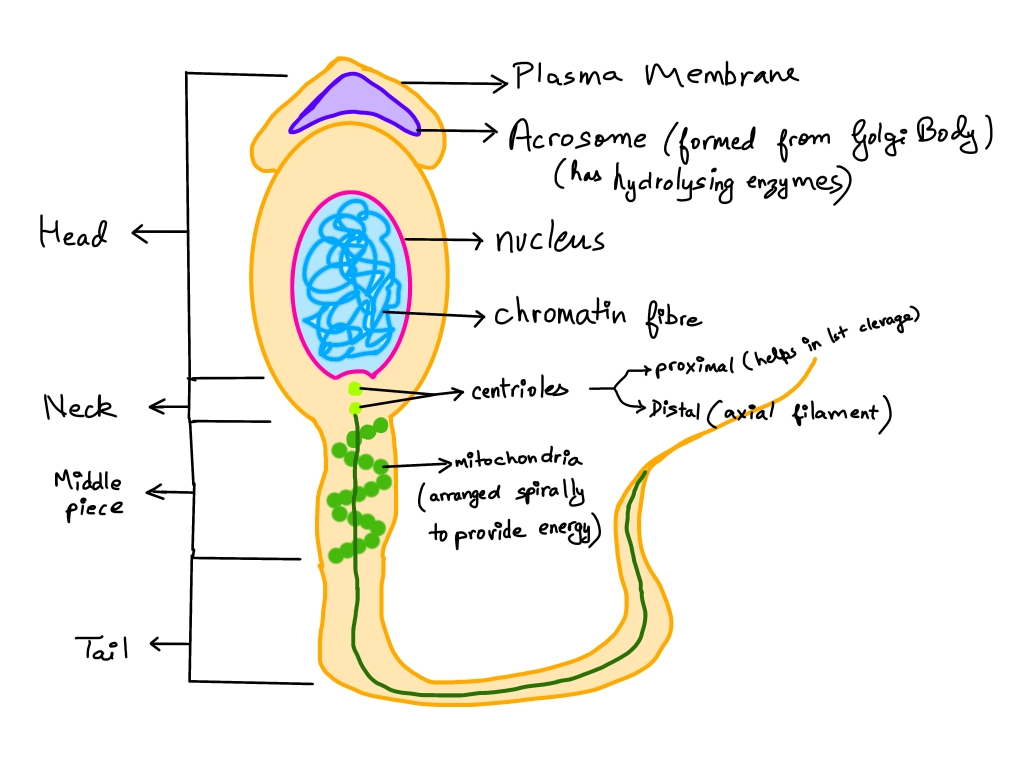
- Structure of Sperm:
- Head:
- Contains the nucleus with haploid DNA (23 chromosomes).
- The acrosome covers the head and contains hydrolytic enzymes (e.g., hyaluronidase, acrosin), which help in penetrating the egg’s zona pellucida during fertilization.
- Neck:
- Connects the head and midpiece.
- Contains the proximal centriole, which is involved in forming the spindle during the first mitotic division of the zygote.
- Midpiece:
- Contains mitochondria, which generate ATP for sperm motility.
- The axoneme (central structure) runs through the midpiece and tail, aiding in movement.
- Tail (Flagellum):
- A long, slender structure responsible for sperm motility.
- Contains microtubules arranged in a 9+2 pattern.
- Propels the sperm forward by whipping motions.
- Function of Sperm:
- Fertilization: Delivers haploid DNA to the ovum.
- Motility: The tail enables the sperm to swim toward the ovum.
- Enzyme Action: The acrosome releases enzymes to penetrate the egg’s outer layer.
✅ 1. Menstrual Cycle: Overview
The menstrual cycle is a 28-day reproductive cycle in females of reproductive age, which prepares the body for potential pregnancy. It involves a series of hormonal, structural, and functional changes in the female reproductive system. The cycle starts at menarche (around 11-14 years of age) and continues until menopause (around 45-50 years of age).
- Significance of the Menstrual Cycle:
- Prepares the uterus for implantation of a fertilized egg.
- Facilitates the release of a mature ovum during ovulation.
- Involves the shedding of the endometrial lining if fertilization does not occur.
- Controlled by hormones secreted by the hypothalamus, pituitary gland, and ovaries.
- Duration:
- The typical menstrual cycle lasts 28 days, but it can vary between 21-35 days in some women.
- The cycle consists of four main phases:
- Menstrual Phase (Day 1-5)
- Follicular Phase (Day 1-13)
- Ovulation Phase (Day 14)
- Luteal Phase (Day 15-28)
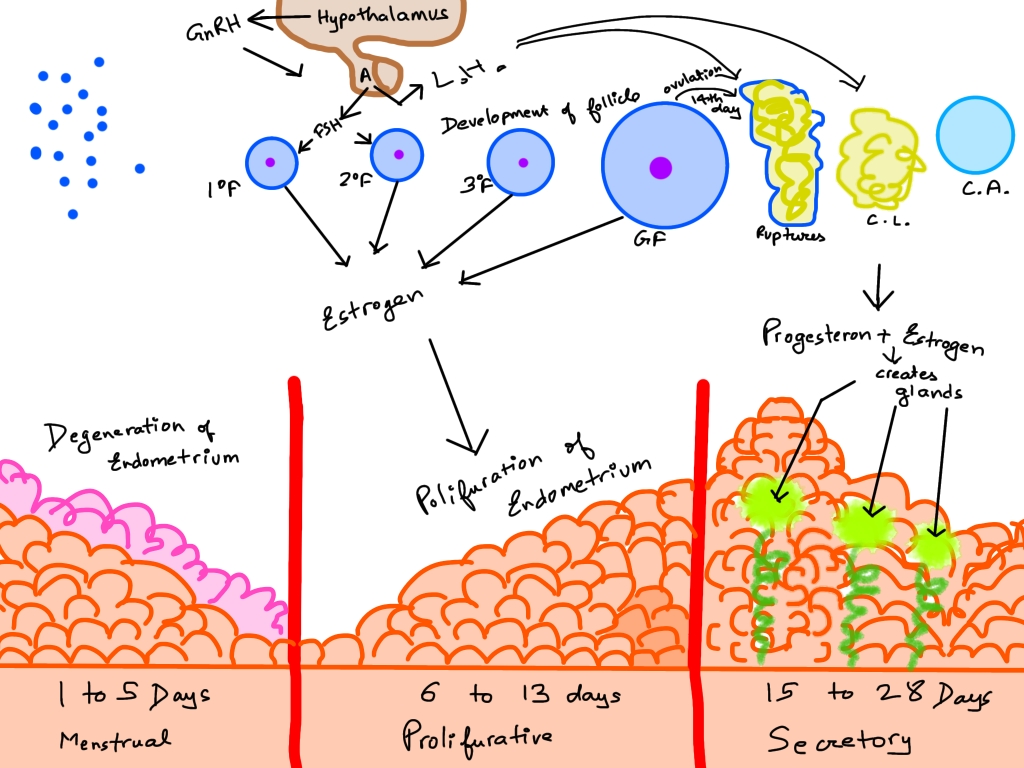
✅ 2. Phases of the Menstrual Cycle
A. Menstrual Phase (Days 1-5)
The menstrual phase marks the beginning of the menstrual cycle and is characterized by the shedding of the endometrial lining.
- Hormonal Changes:
- A drop in progesterone and estrogen levels triggers the shedding of the endometrial lining.
- The decline in progesterone causes the constriction of spiral arteries, reducing blood flow to the endometrium, resulting in its breakdown.
- Physical Changes:
- The endometrial tissue, blood, and mucus are discharged through the vagina as menstrual flow.
- The menstrual flow typically lasts for 3-5 days.
- Symptoms:
- Abdominal cramps due to uterine contractions.
- Lower back pain, fatigue, and mood swings.
B. Follicular Phase (Proliferative Phase) (Days 1-13)
The follicular phase begins on Day 1 of the cycle and lasts until ovulation. It is characterized by the maturation of ovarian follicles and the rebuilding of the endometrium.
- Hormonal Changes:
- The hypothalamus releases gonadotropin-releasing hormone (GnRH), stimulating the pituitary gland to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
- FSH stimulates the growth of ovarian follicles.
- The developing follicles produce estrogen, which causes the thickening of the endometrium.
- Ovarian Changes:
- Several primordial follicles start maturing, but only one dominant follicle (the Graafian follicle) fully matures.
- The follicle secretes estrogen, which causes the endometrial lining to proliferate.
- Uterine Changes:
- The endometrium thickens and becomes rich in blood vessels to prepare for potential implantation.
- Glands and blood vessels proliferate.
- Symptoms:
- Increased vaginal discharge.
- Rise in basal body temperature.
C. Ovulation Phase (Day 14)
The ovulation phase occurs around the 14th day of the cycle and involves the release of a mature ovum from the ovary into the fallopian tube.
- Hormonal Changes:
- A sharp rise in LH levels, known as the LH surge, triggers ovulation.
- FSH levels also increase slightly.
- The estrogen level peaks just before ovulation, promoting the LH surge.
- Ovarian Changes:
- The Graafian follicle ruptures, releasing a secondary oocyte into the fallopian tube.
- The ovum is surrounded by the corona radiata and zona pellucida, which protect it during fertilization.
- Uterine Changes:
- The endometrium is at its thickest and most vascularized, ready for implantation.
- Symptoms:
- Mittelschmerz pain: Mild pelvic pain on one side.
- Increased libido due to hormonal changes.
- A slight increase in body temperature.
- The cervical mucus becomes clear, thin, and stretchy, aiding sperm motility.
- Fertilization Window:
- The ovum survives for 12-24 hours, making this the most fertile period of the cycle.
D. Luteal Phase (Days 15-28)
The luteal phase begins after ovulation and continues until the onset of menstruation. It is marked by the secretion of progesterone and the formation of the corpus luteum.
- Hormonal Changes:
- After ovulation, the ruptured follicle transforms into the corpus luteum, which secretes progesterone and some estrogen.
- Progesterone helps maintain the endometrial lining for implantation.
- If fertilization does not occur, the corpus luteum degenerates into the corpus albicans, causing a drop in progesterone and estrogen levels, triggering menstruation.
- Ovarian Changes:
- The corpus luteum reaches its maximum size by Day 21.
- It produces hormones to support pregnancy if fertilization occurs.
- Uterine Changes:
- The endometrium thickens further and becomes more glandular.
- The glands secrete nutrients to nourish the potential embryo.
- If no fertilization occurs, the endometrial lining begins to break down, initiating the next menstrual phase.
- Symptoms:
- Premenstrual symptoms (PMS):
- Bloating, mood swings, and breast tenderness.
- Fatigue, headaches, and irritability.
- Basal body temperature remains elevated due to high progesterone levels.
- Fertilization Outcome:
- If fertilization occurs, the zygote implants into the endometrium around Day 20-24.
- The developing embryo releases human chorionic gonadotropin (hCG), which maintains the corpus luteum, ensuring continued progesterone production.
- If no implantation occurs, menstruation begins.
✅ 3. Hormonal Regulation of the Menstrual Cycle
The menstrual cycle is regulated by a complex interaction of hormones secreted by the hypothalamus, pituitary gland, and ovaries.
- Hypothalamus:
- Secretes GnRH, which stimulates the pituitary gland to release FSH and LH.
- Pituitary Gland:
- FSH: Stimulates follicle growth and estrogen production.
- LH: Triggers ovulation and the formation of the corpus luteum.
- Ovarian Hormones:
- Estrogen: Promotes the thickening of the endometrium during the follicular phase.
- Progesterone: Maintains the endometrium during the luteal phase.
- Negative Feedback Loop:
- Rising estrogen and progesterone levels inhibit FSH and LH secretion, regulating the cycle.
- Positive Feedback Loop:
- Estrogen stimulates LH surge, triggering ovulation.
✅ 1. Fertilization: Overview
Fertilization is the fusion of a haploid male gamete (sperm) with a haploid female gamete (ovum) to form a diploid zygote. It typically occurs in the ampullary region of the fallopian tube, which is the most common and favorable site for fertilization.
- Significance of Fertilization:
- Restores the diploid chromosome number (46 chromosomes in humans).
- Combines genetic material from both parents, creating genetic diversity.
- Activates the developmental process, leading to the formation of the embryo.
✅ 2. Steps of Fertilization
A. Sperm Transport and Capacitation:
- After ejaculation, sperm are deposited in the vagina and travel through the cervix, uterus, and fallopian tubes.
- Only a few hundred sperm (out of millions) reach the ampullary region.
- During this journey, sperm undergo capacitation, a process that takes 5-6 hours.
- Capacitation:
- The membrane covering the acrosome becomes thinner.
- The sperm become hyperactive and motile, enhancing their ability to penetrate the ovum.
B. Binding of Sperm to Ovum:
- The ovum is surrounded by two protective layers:
- Corona radiata: Outer layer made of follicular cells.
- Zona pellucida: Inner glycoprotein layer surrounding the oocyte.
- Sperm bind to receptors (ZP3 glycoprotein) on the zona pellucida.
- This binding initiates the acrosomal reaction.
C. Acrosomal Reaction:
- The acrosome in the sperm head releases hydrolytic enzymes such as:
- Hyaluronidase: Breaks down the corona radiata.
- Acrosin and proteases: Digest the zona pellucida, allowing the sperm to reach the oocyte.
D. Penetration and Fusion:
- Once a sperm penetrates the zona pellucida, it reaches the perivitelline space (between zona pellucida and oocyte membrane).
- The sperm’s plasma membrane fuses with the oocyte’s membrane.
- The sperm nucleus and centrioles enter the ovum’s cytoplasm.
- The ovum completes meiosis-II, forming a haploid female pronucleus and a second polar body.
- The male and female pronuclei fuse, forming a diploid zygote (2n).
E. Prevention of Polyspermy:
- Polyspermy (fertilization by multiple sperm) is prevented by two mechanisms:
- Fast Block: The oocyte membrane undergoes depolarization immediately after sperm entry, preventing additional sperm from binding.
- Slow Block (Cortical Reaction): Cortical granules release enzymes that harden the zona pellucida, making it impermeable to other sperm.
✅ 3. Implantation: Overview
Implantation is the process by which the blastocyst attaches to the endometrial lining of the uterus. It occurs about 6-7 days after fertilization.
- Significance of Implantation:
- Anchors the developing embryo to the uterine wall.
- Establishes nutritional and hormonal communication with the maternal tissues.
- Initiates the formation of the placenta.
✅ 4. Steps of Implantation
A. Development of the Blastocyst:
- After fertilization, the zygote undergoes cleavage to form a morula (a solid ball of 16-32 cells).
- The morula develops into a blastocyst, consisting of:
- Trophoblast: Outer layer that forms the placenta.
- Inner Cell Mass (ICM): Develops into the embryo.
- Blastocoel: Fluid-filled cavity.
- The zona pellucida degenerates before implantation, allowing the blastocyst to attach to the uterine wall.
B. Attachment and Invasion:
- The blastocyst adheres to the endometrium (usually in the upper posterior wall of the uterus).
- The trophoblast differentiates into two layers:
- Cytotrophoblast: Inner layer that forms the structure of the placenta.
- Syncytiotrophoblast: Outer layer that invades the endometrial tissue and releases enzymes to dissolve part of the uterine lining, enabling implantation.
- The blastocyst becomes partially embedded by Day 6-7 and fully embedded by Day 10-12.
C. Formation of Placenta:
- After implantation, the chorionic villi develop from the trophoblast.
- These villi penetrate the endometrium and establish a connection with maternal blood vessels.
- The placenta forms and facilitates:
- Exchange of gases, nutrients, and waste between the mother and the fetus.
- Secretion of human chorionic gonadotropin (hCG), which maintains the corpus luteum and supports pregnancy.
✅ 5. Hormonal Regulation of Implantation
- Progesterone:
- Prepares the endometrium by promoting vascularization and glandular secretion.
- Maintains the uterine lining during pregnancy.
- Estrogen:
- Stimulates the proliferation of the endometrial lining, preparing it for implantation.
- hCG (Human Chorionic Gonadotropin):
- Secreted by the trophoblast after implantation.
- Sustains the corpus luteum, which continues to produce progesterone until the placenta takes over.
✅ 1. Pregnancy: Overview
Pregnancy is the physiological state in which a fertilized egg develops into a fetus inside the uterus of the mother. It lasts for approximately nine months (40 weeks) or 280 days, divided into three trimesters, each marked by specific developmental milestones.
- Stages of Pregnancy:
- Fertilization: Fusion of sperm and ovum to form a zygote.
- Implantation: The blastocyst attaches to the uterine wall, forming the placenta.
- Gestation: The period of fetal development in the uterus.
- Parturition: The expulsion of the baby from the mother’s uterus.
- Hormonal Regulation of Pregnancy:
- hCG (Human Chorionic Gonadotropin):
- Produced by the trophoblast after implantation.
- Maintains the corpus luteum, ensuring continued progesterone production to sustain the uterine lining.
- Progesterone:
- Maintains the thickness and vascularization of the endometrium.
- Inhibits uterine contractions, preventing miscarriage.
- Estrogen:
- Promotes the growth of the uterine lining.
- Stimulates the development of the mammary glands.
- Relaxin:
- Relaxes the pelvic ligaments and widens the cervix in preparation for childbirth.
- Placental Hormones:
- After the corpus luteum degenerates, the placenta takes over the secretion of progesterone and estrogen.
- Duration of Pregnancy:
- First trimester: 1-12 weeks → Formation of major organs.
- Second trimester: 13-27 weeks → Fetal growth and development.
- Third trimester: 28-40 weeks → Final growth and preparation for birth.
✅ 2. Embryonic Development: Overview
Embryonic development refers to the series of cell divisions and differentiation events that transform the zygote into a complex multicellular organism. It occurs during the first eight weeks of pregnancy.
✅ 3. Stages of Embryonic Development
A. Zygote Formation:
- After fertilization, the zygote (a single diploid cell) forms.
- It begins to undergo mitotic divisions.
B. Cleavage:
- Rapid mitotic divisions of the zygote without increasing in size.
- Results in the formation of a morula (16-32 cells).
- The morula travels through the fallopian tube towards the uterus.
C. Blastulation:
- The morula transforms into a blastocyst.
- The blastocyst consists of:
- Trophoblast: Outer layer that forms the placenta.
- Inner Cell Mass (ICM): Becomes the embryo.
- Blastocoel: Fluid-filled cavity.
- The blastocyst implants into the endometrium.
D. Gastrulation:
- The blastocyst differentiates into three germ layers:
- Ectoderm: Forms the nervous system, skin, and sensory organs.
- Mesoderm: Develops into the musculoskeletal system, circulatory system, kidneys, and reproductive organs.
- Endoderm: Forms the digestive system, liver, pancreas, and lungs.
E. Neurulation:
- The formation of the neural tube, which gives rise to the brain and spinal cord.
- Marks the beginning of the nervous system development.
F. Organogenesis:
- Formation of vital organs from the germ layers.
- By the end of the eighth week, the embryo has all major organs and structures.
- The embryo is now referred to as a fetus.
✅ 4. Features of Embryonic Development
A. Germ Layer Formation:
- The ectoderm, mesoderm, and endoderm differentiate into specific tissues and organs.
- This process is essential for the formation of complex organ systems.
B. Morphogenesis:
- Involves the shaping of the embryo by tissue and organ formation.
- The body plan of the organism becomes evident.
C. Differentiation:
- Specialized cells arise from unspecialized cells.
- Cells take on distinct forms and functions.
- Example: Muscle cells, nerve cells, and skin cells differentiate from the germ layers.
D. Growth and Development:
- The embryo increases in size and complexity.
- The nervous system, heart, and limbs begin to form.
E. Fetal Membranes Formation:
- Four fetal membranes form to support the embryo:
- Amnion: Encloses the embryo and contains amniotic fluid, which protects it from shocks.
- Chorion: Forms the outer membrane and contributes to the placenta.
- Yolk Sac: Produces blood cells during early development.
- Allantois: Involved in the formation of the umbilical cord.
✅ 5. Parturition: The Process of Childbirth
Parturition is the process of expelling the fetus from the uterus at the end of pregnancy. It is triggered by hormonal and mechanical factors.
A. Hormonal Regulation:
- Oxytocin:
- Secreted by the posterior pituitary.
- Stimulates uterine contractions during labor.
- Causes the cervix to dilate and promotes the release of prostaglandins, enhancing contractions.
- Relaxin:
- Softens the cervix and loosens the pelvic ligaments.
- Progesterone Drop:
- Decreases before labor, allowing for stronger uterine contractions.
B. Stages of Parturition:
- Dilation Stage:
- Cervix dilates to around 10 cm.
- Lasts 6-12 hours in first-time mothers.
- Expulsion Stage:
- Strong contractions push the baby through the birth canal.
- Lasts for 20-60 minutes.
- Placental Stage:
- After the baby is delivered, the placenta is expelled.
- Takes around 15-30 minutes.
✅ 6. Lactation: Milk Production and Secretion
Lactation is the process by which the mammary glands produce and secrete milk to nourish the newborn.
A. Hormonal Control:
- Prolactin:
- Secreted by the pituitary gland.
- Stimulates milk production in the mammary glands.
- Oxytocin:
- Stimulates the ejection of milk from the mammary glands during suckling.
B. Colostrum:
- The first milk secreted after childbirth.
- Rich in antibodies, proteins, and nutrients.
- Provides immunity and protection to the newborn.
C. Importance of Breastfeeding:
- Provides optimal nutrition for the baby.
- Strengthens the immune system through maternal antibodies.
- Promotes bonding between mother and baby.
- Reduces the risk of infections and allergies.